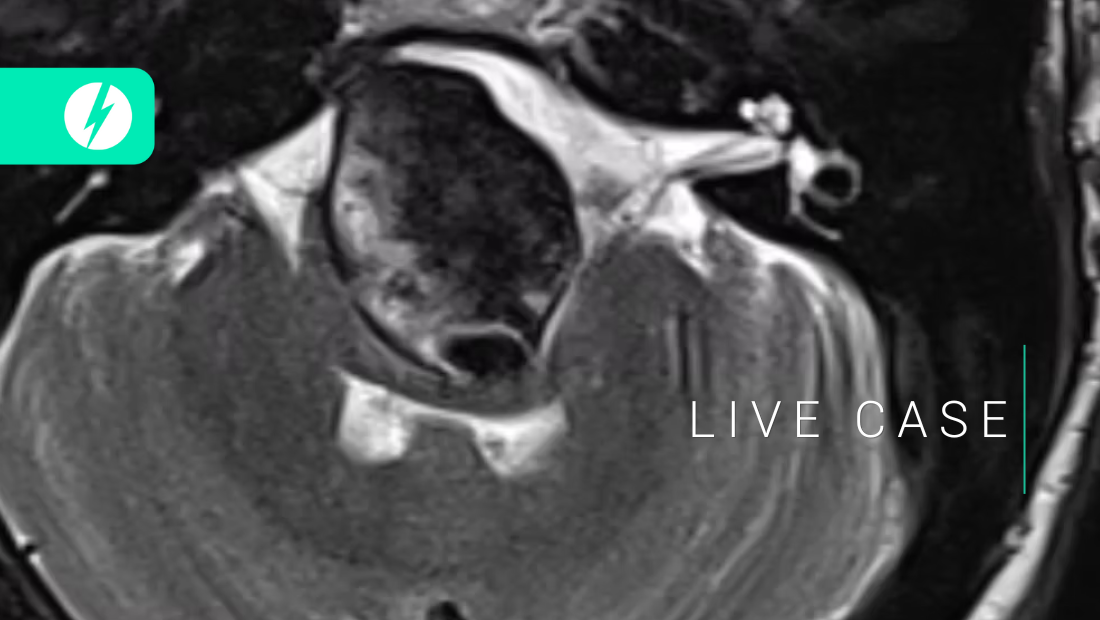
LIVE CASE
13
episodes

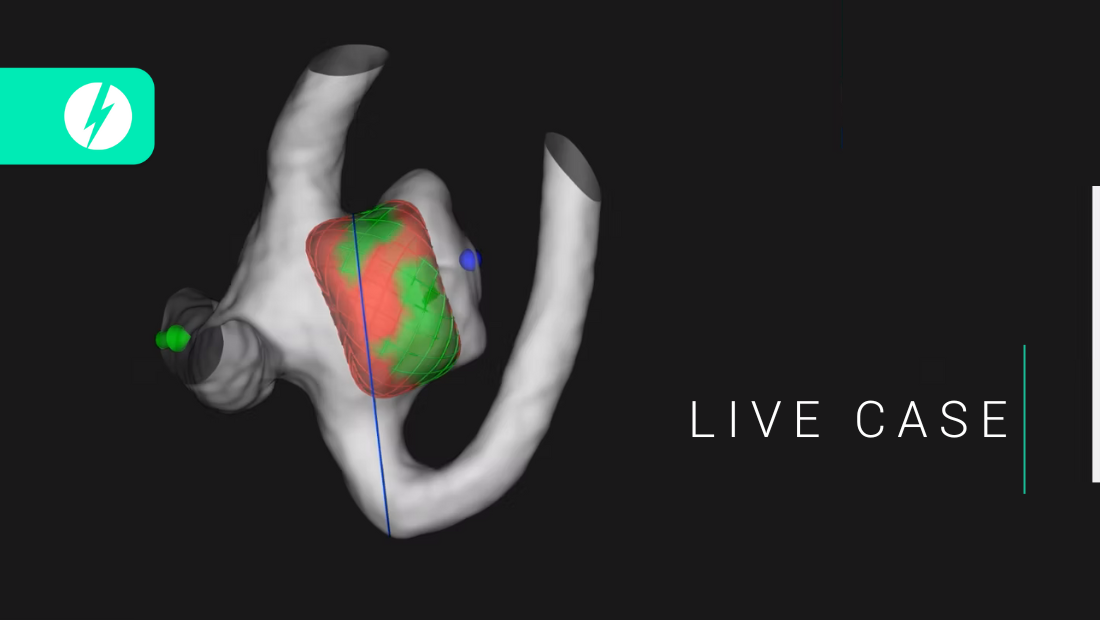
Extradural giant aneurysms - SLICE Next Frontiers 2022 - Greta REIKONEN

Giant cavernous aneurysm treatment - SLICE Next Frontiers 2022 - Lucy HARRYS

Yves Moulin & Paulina Hachette - SLICE Next Frontiers 2022

Recanalization of top-of-the basilar aneurysms after simple coiling - SLICE Next Frontiers 2022 - Samantha BIDOO
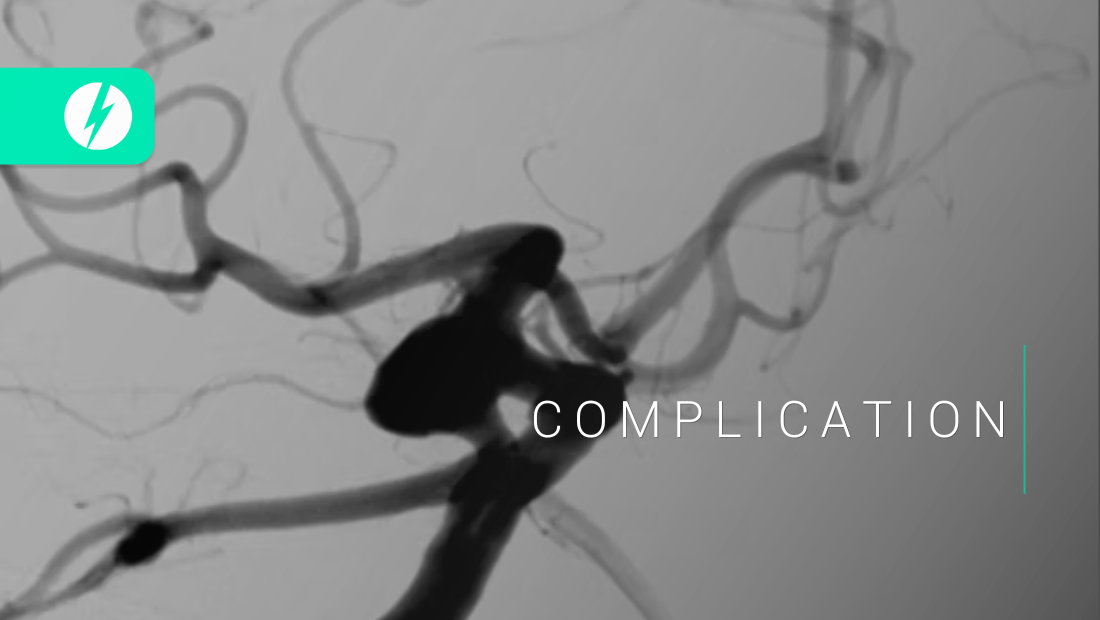
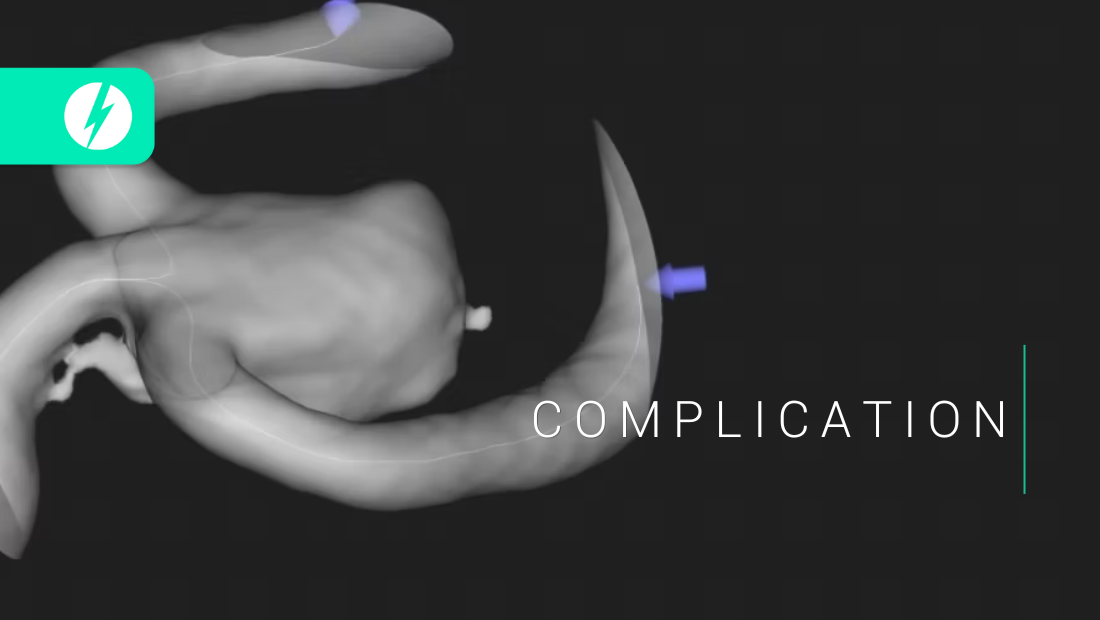
Fish-mouthing of a stent and how to deal with it - SLICE Next Frontiers 2022 - Maria CHOCALHO - Medhi TYRE

Alexandro Pretro - SLICE Next Frontiers 2022
David Plateau - SLICE Next Frontiers 2022

Endovascular treatment of MCA - SLICE Next Frontiers 2022 - Julien CIAGAR
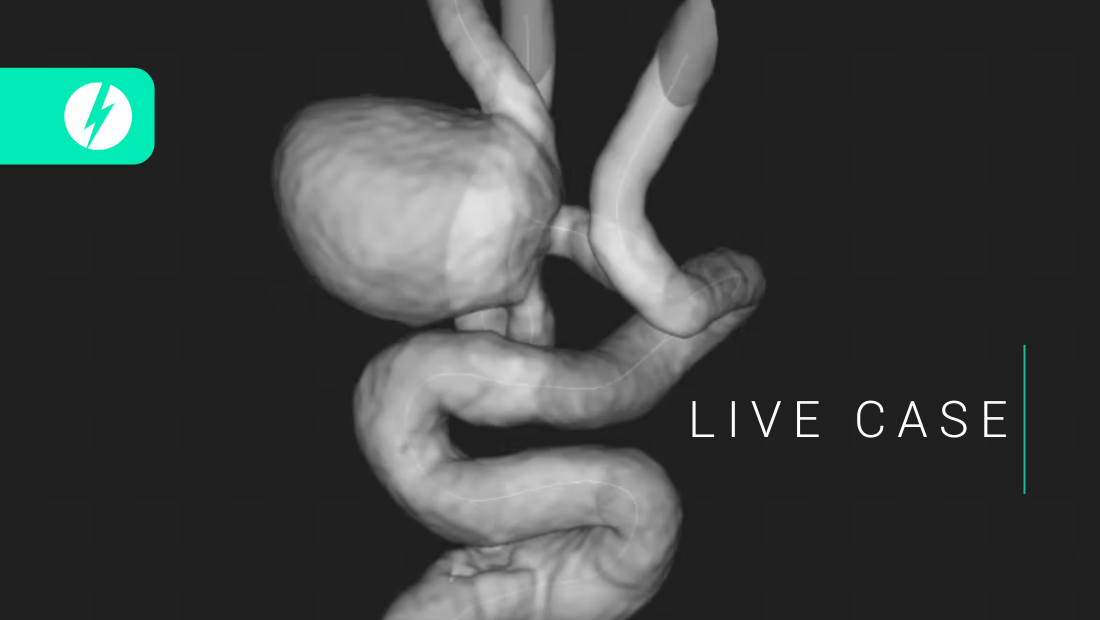
10mm size MCA aneurysm - SLICE Next Frontiers 2022 - Annie JOB
Axel Bilbon - SLICE Next Frontiers 2022
Tips and tricks to deal with branch protrusions - SLICE Next Frontiers 2022

Wide neck-bifurcation aneurysms - SLICE Next Frontiers 2022
