M1 Thrombectomy - SLICE Worldwide 2022
Best techniqueHow to perform an M1 - Thrombectomy
Introduction:
Thrombectomy has been around for several years. Pioneering centers started in 2008-2009, and it became a routine procedure in the developed world with the completion of the big thrombectomy trials in 2015, as opposed to initial thrombectomies performed with the Solitaire stent using 6Fr guiding catheters – the procedure evolved and improved, in parallel with newer materials that were added to the market. Today, there are several techniques, each bearing a fancy name and claiming theoretical supremacy. However, several randomized trials and retrospective data sets have not proven a clear benefit on 3-month outcomes for specific techniques. They manage, however, to show differences in first-pass effects and rates of TICI 3, and this literature should be consulted and interpreted by all interventionalist currently treating acute ischemic stroke.
As clearly demonstrated in the discussion accompanying this technical video, clinicians have no consensus about the optimal technicalities of the typical M1 thrombectomy. Still, several key factors should be considered by the young practitioner.
Several technics:
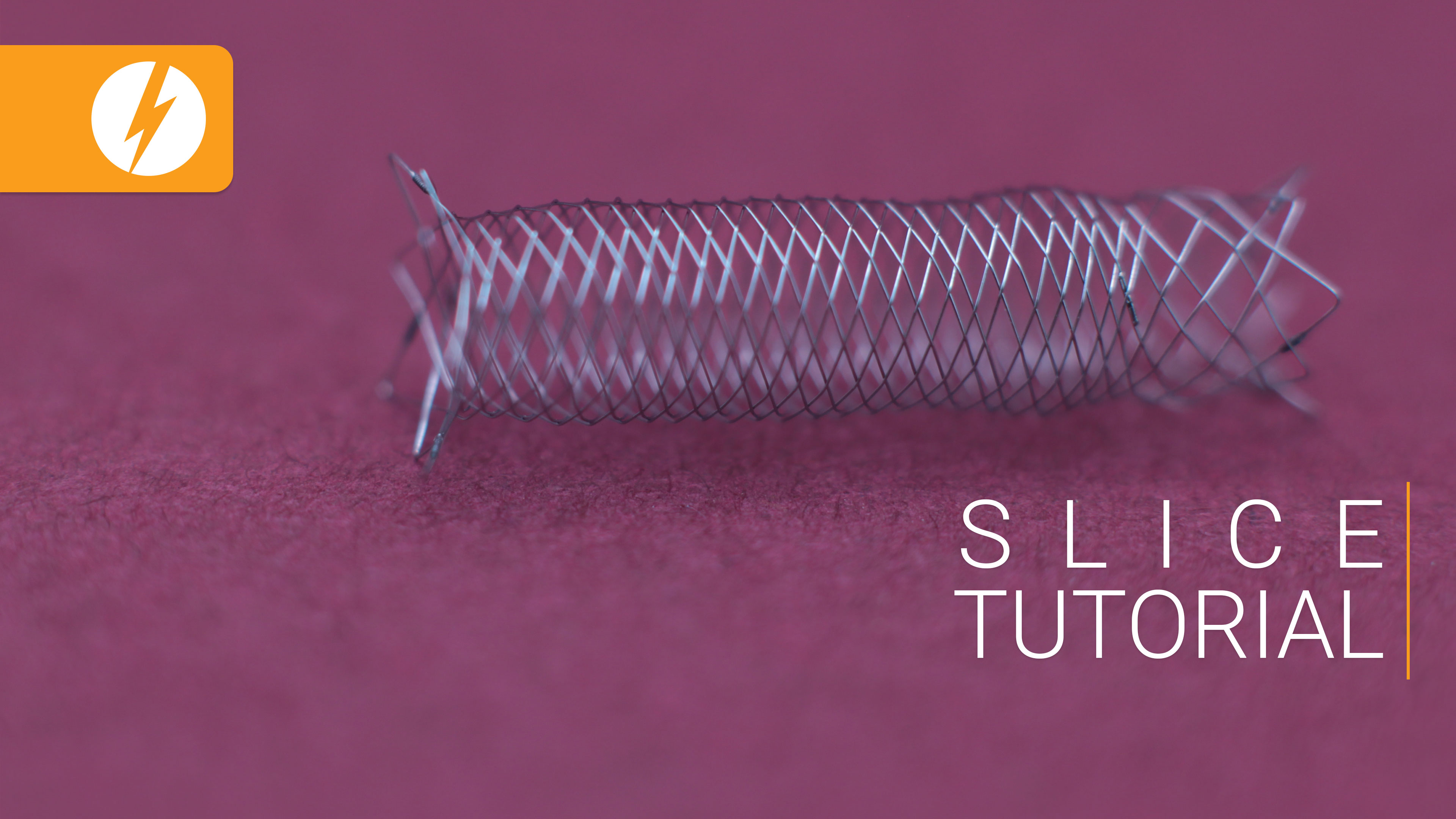
ADAPT – A Direct Aspiration First Pass Technique:
A large-bore aspiration catheter is advanced to the proximal aspect of the thrombus and connected to a source of continuous aspiration, and the thrombus is suctioned.
Theoretical advantage:
- Direct thrombus aspiration has the advantage over the stent retriever technique in that the thrombus does not have to be passed
- Cheaper as no stent-retriever is used
Theoretical disadvantage:
- Fragmentation of the distal part of the thrombus and higher risk of distal emboli and incomplete TICI 3
- Difficulties in tracking the distal aspiration catheters to the desired location
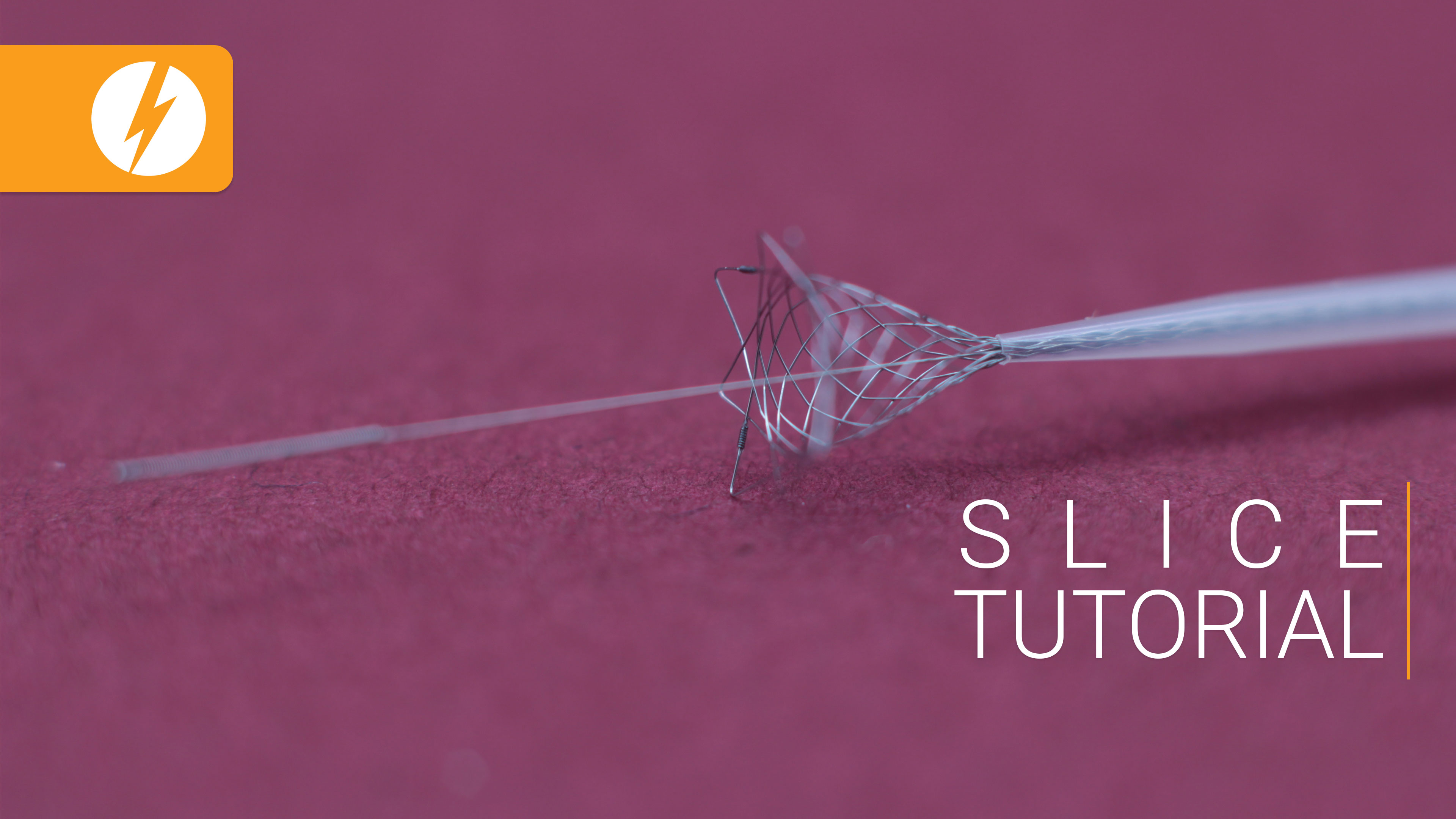
SAVE - Stent Retriever Assisted Vacuum locked Extraction:
The thrombus is removed with a stent retriever under continuous aspiration. The stent retriever is fixing the thrombus to the aspiration catheter, which is withdrawn with continuous aspiration and additional aspiration of the guiding catheter
Theoretical advantage:
- Less risk of distal thrombus and emboli. The stent-retriever acts as a “filter”.
- Higher rates TICI 3 and first-pass effect
Theoretical disadvantage:
- More costly.
- More complicated.
STAR - Solitaire Flow Restoration Thrombectomy for Acute Revascularization:
The Solitaire Flow Restoration device is a self-expanding stent retriever. When the stent is deployed within the target clot in the occluded vessel, the stent struts entrap the thrombus. When the stent is withdrawn in its unfolded state, the enmeshed thrombus is concurrently extracted from the vessel.
Theoretical advantage:
- No aspiration catheter is needed. Microcatheters are easier to navigate.
- Less costly than a combined technique.
- Can be changed to double stent-retriever technique if several passes are unsuccessful.
Theoretical disadvantage:
- Less effective than the SAVE technique
- Much less effective if a balloon guide is not used.
Conclusion
The chosen technique depends on several factors such as experience, familiarity with different devices, and reimbursement and will always be adapted to the situation by the treating physician. The accompanying video is a great theoretical resource for optimizing key steps of the combined stent-retriever aspiration technique. Regardless of what center preferences exist for M1 – thrombectomy, knowledge about the optimal use of stent-retrievers, aspiration catheters, and especially balloon-guide catheters should be sought by each interventionalist. Rapid adaptability by the interventionalist and comparison of local to published results should be employed. The technique will constantly evolve in the future, and we must keep up with device improvements to offer the majority of our patients the best chance of timely M1 – distal emboli-free full recanalization with a first-pass.