Bifurcation MCA Occlusion
Double stent retriever technique – how and when to perform it?
Introduction:
Mechanical thrombectomy using double stent retriever technique involves deployment of two stent-retrievers side by side into the clot at the arterial bifurcation and retrieval as a single unit.
The double stent retriever technique may be particularly helpful for refractory clots involving arterial bifurcation and used as bailout strategy when the clot is resistant to multiple passes of a single stent retriever technique or as a first line strategy when there is an evidence of saddle thrombus in imaging and co-dominance of the two involved branches.
With this technique, there is a greater possibility of clot’s removal, because it allows more coverage of the thrombus within the stent struts and may lead to better outcomes1.
When to perform it?
Saddle thrombus in ICA bifurcation, MCA M1/M2 bifurcation, basilar bifurcation
Types of the techniques:
Simultaneous double stent-retrievers technique
Crossing double stent-retrievers technique
How to perform it?
Simultaneous double stent-retrievers technique
1. Make sure that you are using long introducer/balloon guide catheter enabling simultaneous insertion of two microcatheters (both 0,021 inch or eventually one 0,021 and one 0,017 inch).
2. Whenever it is possible, try to use distal access catheter (DAC) that you will place in contact with the front of the thrombus, but without dragging it too hard, so you avoid pinching of the artery and further damage to arterial wall. The minimal inner lumen diameter of DAC that allows usage of two 0,021 inch microcatheter is 0,070 inch.
3. Go with the first microcatheter to the first branch. There are no recommendations regarding the order in which branch catheterization should be performed, you can start with the branch wherever your microwire go first or with the branch which seems to be more difficult to catheterize.
4. Go with the second microcatheter to the second branch. Be aware of shipping effect which can make catheterization of the second branch more difficult.
5. Insert the stent-retrievers to both of your microcatheters and position them at the tip of the catheters.
6. You may open up the stent-retrievers simultaneously or one after each other.
7. It is very important to properly choose your stent-retriever’s size:
Stent-retrievers of two different sizes can be use.
Longer the stent-retriever is, better the result. It is especially important that the first stent-retriever should be as long as possible.
Larger diameter stent-retrievers lead to higher reperfusion rates but also are associated with higher prevalence of hemorrhage. A 6 mm diameter first stent-retriever independently predicts more intracranial hemorrhages. For more information check-up the publication below2.
8. Once the stent-retrievers are deployed, remove the microcatheters to enhance the aspiration surface for DAC.
9. Retrieve the two stent-retrievers and DAC as one-piece unit on continuous aspiration.
Crossing double stent-retrievers technique
1. You may use smaller diameter long introducer/ balloon guide catheter because there will be only one microcatheter inserted at the same time.
2. You may use smaller diameter distal access catheter (DAC) because there will be only one microcatheter inserted at the same time.
3. Go with the first microcatheter to the first branch. There are no recommendations regarding the order in which branch catheterization should be performed, you can start with the branch wherever your microwire go first or with the branch which seems to be more difficult to catheterize.
4. Deploy the stent-retriever in the first branch.
5. Cross the previously deployed stent-retriever and catheterize the second branch with the microcatheter.
6. Deploy the second stent-retriever in the second branch.
7. Use the same stent-retriever’s selection criteria as discussed in the technique above.
8. Once the stent-retrievers are deployed, remove the microcatheters to enhance the aspiration surface for DAC.
9. Retrieve the two stent-retrievers and DAC as one-piece unit on continuous aspiration.
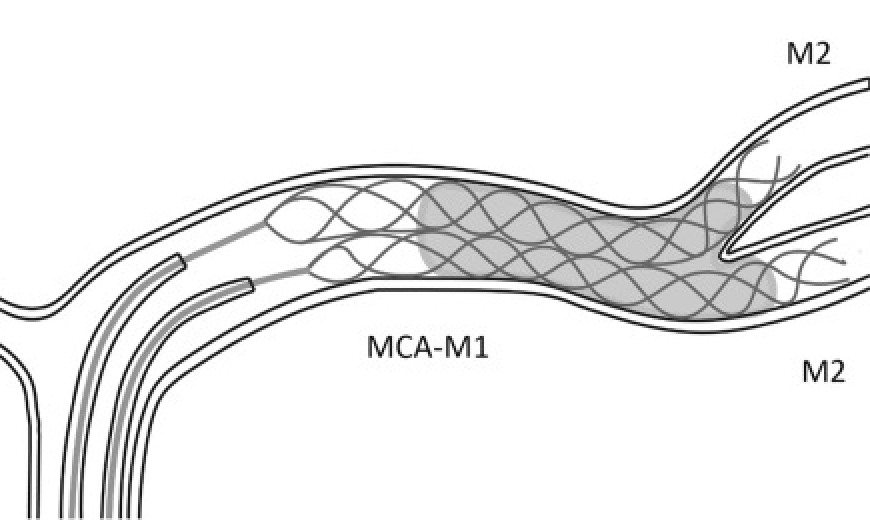
Simultaneous double stent-retrievers technique 1
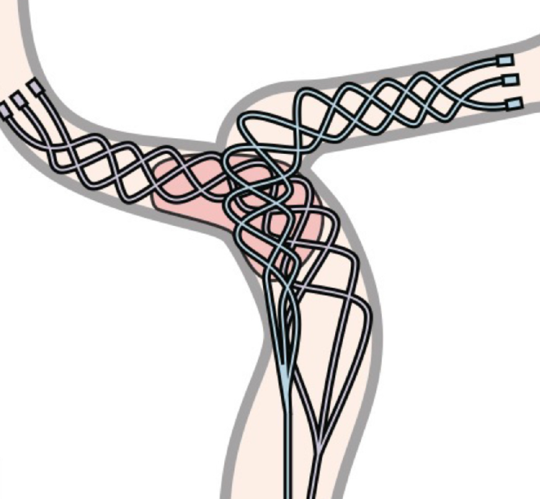
Crossing double stent-retrievers technique 4
Remarks:
- Double stent-retrievers technique increase about 1.4 times endothelial damage compare to single stent-retriever technique3.
- Traction (retrieval force) in double stent-retrievers technique is much higher than in one stent-retriever technique so there is a higher risk of disruption of perforators and hemorrhage. For this reason the technique is reserved for proximal occlusions and the usage of distal access catheter to compensate the vector of the forces is recommended.
- Crossing double stent-retrievers technique rely on trapping of the second stent within the first one so the shear stress during retrieval is more important and may lead to higher prevalence of endothelial damage and hemorrhage.
Conclusions:
The double stent-retievers technique is effective in saddle bifurcation and refractory thrombus, but may be associated with an increased risk of endothelial damage and hemorrhage, so to be safe, must be used in carefully defined cases with caution.
Literature:
1. Patro, Satya Narayana, and Daniela Iancu. "Dual-stent retrieval for mechanical thrombectomy of refractory clot in acute stroke as a rescue technique." Cmaj 189.17 (2017): E634-E637.
2. Cabral, Lucas Scotta, et al. "Device size selection can enhance Y-stentrieving efficacy and safety as a rescue strategy in stroke thrombectomy." Journal of NeuroInterventional Surgery 14.6 (2022): 558-563.
3. Hernández, David, et al. "Increased Number of Passes and Double Stent Retriever Technique Induces Cumulative Injury on Arterial Wall After Mechanical Thrombectomy in a Swine Model." Translational stroke research (2022): 1-9.
4. Sasaki, Isao, et al. "Crossing double stent retriever technique for refractory terminal internal carotid artery occlusion." Radiology Case Reports 17.6 (2022): 1848-1852.



