Pulsatile Tinnitus : epidemio, symptoms, etiologies and treatment - SLICE Next Frontiers 2023
Live CasePulsatile tinnitus – the awaken nightmare
• Introduction:
- Pulsatile tinnitus (PT) is a symptom referred commonly as an unusual rhythmic unwanted hearing sensation. It is related with decreased quality of life and might dysregulate psychiatric conditions, as anxiety and depression. It is also important to remark its impact in suicide rates, which are four times higher in PT affected individuals. Patients can also complain about poor concentration, low self-steam, and insomnia. (1)
- Approximately 10% of all tinnitus are pulsatile, which counts as around 5 million people affected just in US (2). Approximately 70% of PT are due to an underlying identifiable cause. (3)
• Semiology
o General symptoms and clinical history
• It is fundamental to question the patients about their quality of life and its decrease due to PT.
• Asking about the severity of the symptoms and how much they are heard along the day
• Interrogate about early symptoms of intracranial hypertension (Headache, visual impairment, diplopia)
As we can see in the video, general symptoms are most frequently described as:
• Wooshing (Doppler like)
• Synchronized to pulse rate
• Increased by effort
• Decreased at rest
• Modified (commonly decreased) by cervical compression
• Modified by head position
o Physical examination
The video clarifies some of the examination maneuvers that could be clinically performed in order to standardizing clinical examination:
• Simple skull auscultation utilizing a stethoscope
• Requesting the patient to move his/her head upwards, sidewards, and downwards – evaluate any changes in the PT
• Inducing PT increase by stimulating the patient to walk which may temporarily raise intracranial pressure and consequently turn it louder
• Recording PT with specific transcanal microphone devices depending on its frequency (Sensitivity around 15-20%)
• Neurological assessment, including papilledema investigation
1. Important clinical note: Balloon-test occlusion – Might be an option to PT assessment in cases the physician is not convinced that the brain imaging findings are directly responsible for a PT. Then, interventionalists are able to occlude different parts of the anatomy and check if any changes arise.
• Etiology
We can watch in the video that many causes are quote as possible
etiologies for PT – classically they are described as vascular and nonvascular etiologies.
o Vascular
- Arterial
• Atherosclerosis – Intracranial/Cervical stenosis.
• AVMs
• Fistulas
• High blood pressure
• Cervical dissection
- Venous
• Venous stenosis – idiopathic intracranial
hypertension (IIH) -> most common vascular cause
• Sigmoid diverticulum or pouches
• Sinus dehiscence
• Intra-mastoidal vein
o Non-vascular
- Bones
• Paget disease/hypervascularization
• Eagle syndrome at the neck
• Temporal bone structural abnormality
o Semi-circular canal dehiscence
o Diverticulum
o Sinus dehiscence
- Blood/Metabolic
• Anemia
• Hyperthyroidism
• Valvular heart disease
• Medications – Cisplatin/Aminoglycosides (1)
- Tumors/Neoplasia
- Head trauma
• Brain imaging
As shown in the video, in order to standardizing the radiologic assessment to PT, it is indicated the following images modalities
o MRI
• TRICKS or Dynamic gadolinium
• 3D venogram
• Coronal T2
• Flair
• TOF images
• GAD FAT SAT
o CTA head and neck
o 3D angiographic venogram technique: Arterial access (wrist), vascular drainage acquisition, calculation of the delay to veins arising then set the delay in the 3D before performing the next run.
• Treatment
We can check in the video all the multiple modalities of treatments, which include
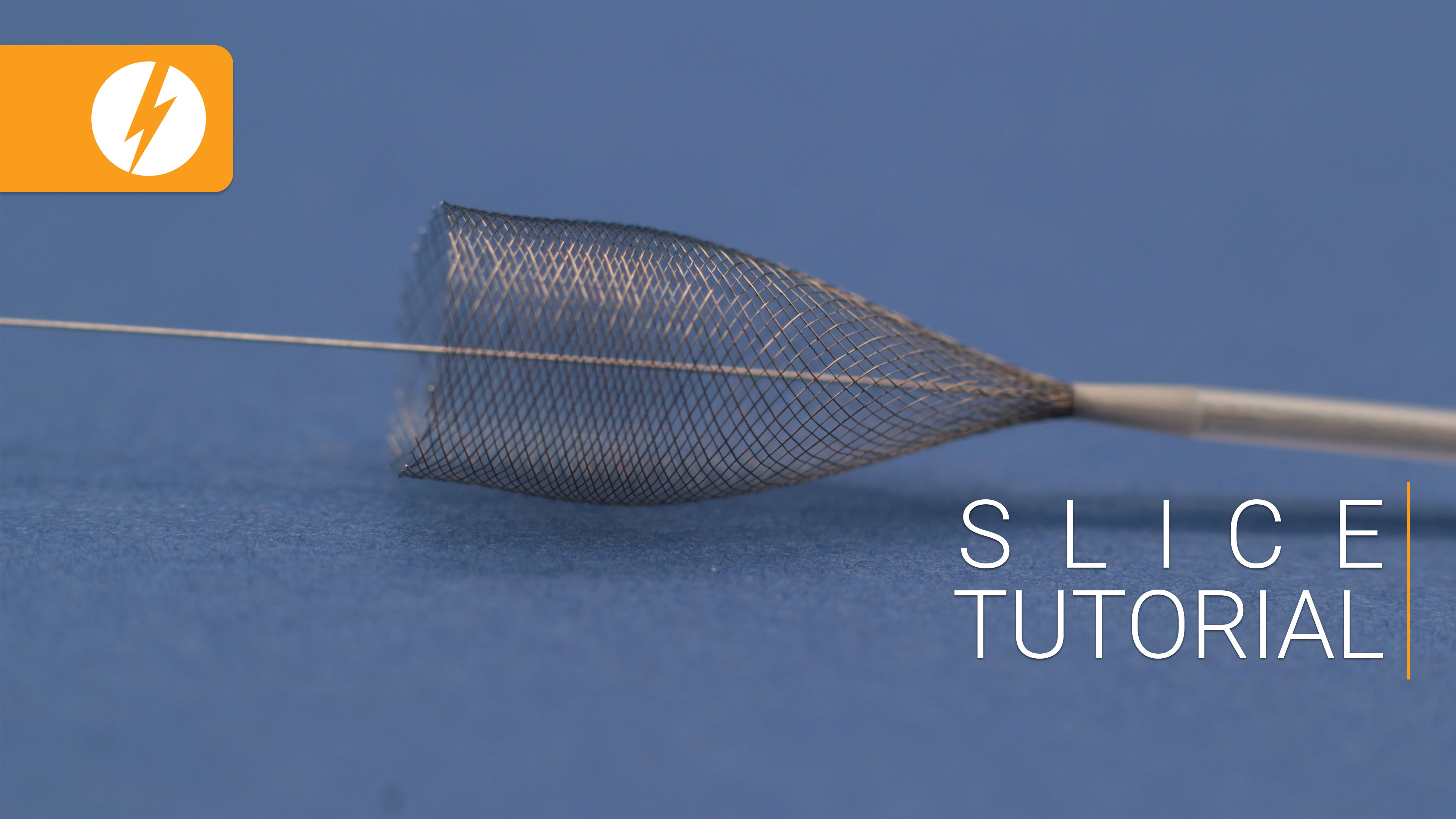
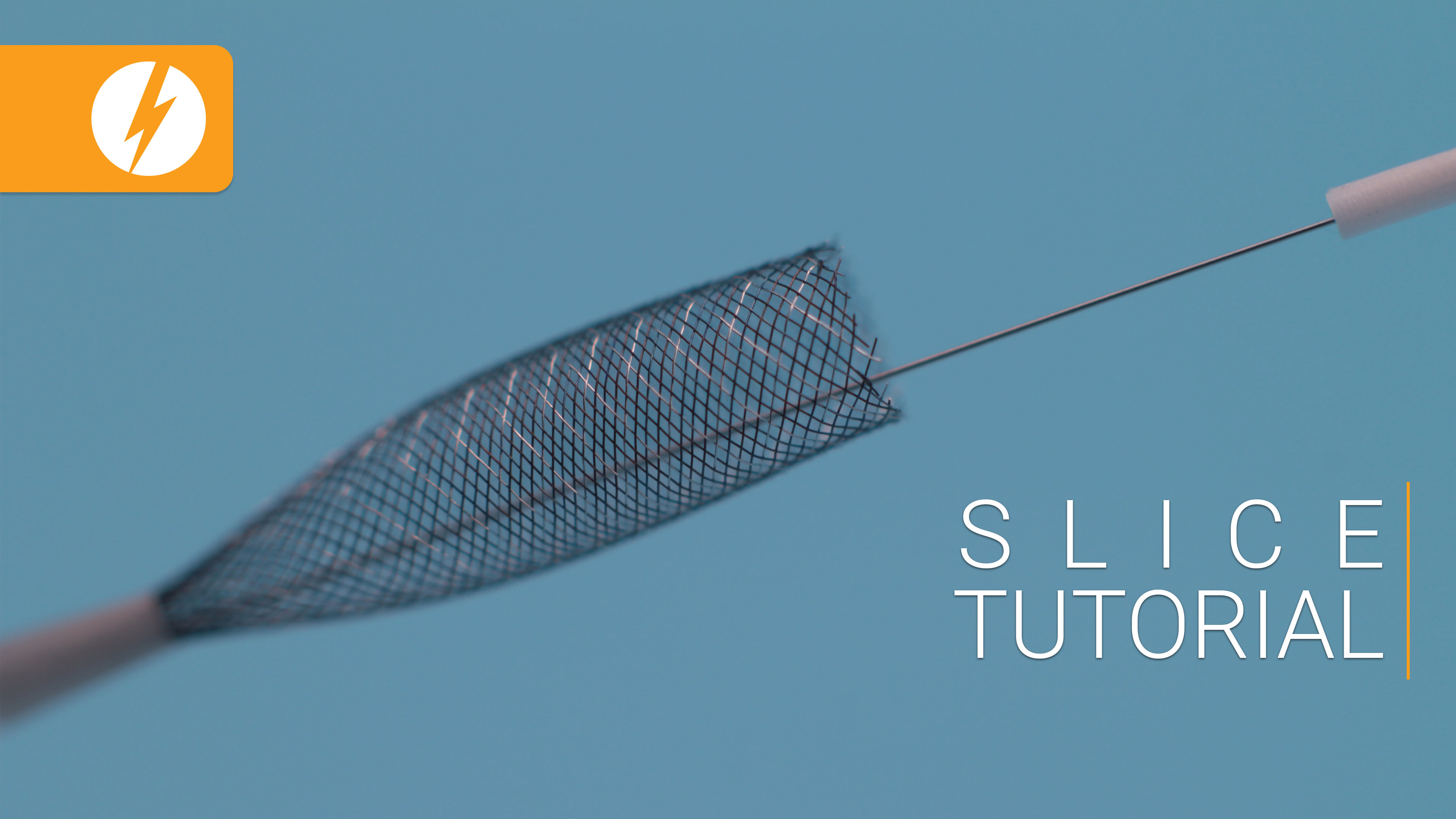
o Stenting of intra or extra-cranial vessels
2. Important clinical note: IIH x PT – There is a clear overlap between these two entities then within patients with PT due to a venous stenosis, for example, it is indicated to place a stent in the venous sinus which may not be same for IIH since there may be a pressure gradient for venous stenting indication.
3. Venous sinus stenting technique (Transverse sinus): Femoral vein access Navian 5f + microcatheter to navigate. Crossing the sigmoid-transverse transition. Insert the stent in the Navian. Reach to the interest area and deploy the stent.
o Surgical treatments for compressive (bones, tumors) causes (3).
Further Reading
1. Kumar R, Rice S, Lingam RK. Detecting causes of pulsatile tinnitus on CT arteriography-venography: A pictorial review. Eur J Radiol. 2021;139:109722.
2. Narsinh KH, Hui F, Duvvuri M, Meisel K, Amans MR. Management of vascular causes of pulsatile tinnitus. J Neurointerv Surg. 2022;14(11):1151-7.
3. Narsinh KH, Hui F, Saloner D, Tu-Chan A, Sharon J, Rauschecker AM, et al. Diagnostic Approach to Pulsatile Tinnitus: A Narrative Review. JAMA Otolaryngol Head Neck Surg. 2022;148(5):476-83.
Video Related